You’re not alone if you have persisting symptoms following infection with COVID. You might also be wondering why. As the research evolves we are beginning to understand more. With this, we hope to be able to offer education and guidance to help you return to health.
From not knowing anyone who had covid to being the odd one out not having it, the increasing number of infections in our community is bringing attention to ongoing health concerns as a result.
Traditionally considered a respiratory illness, most will experience mild symptoms from infection with no ongoing concern. However, there is a cohort of the population remaining symptomatic for weeks to months post the initial infection. Continuing symptoms is often termed long COVID (>12 weeks).
Ongoing symptoms may include, fatigue, chest pain, joint/muscle pain, dizziness, fever, shortness of breath, gastrointestinal symptoms, headache, sore throat, neurocognitive disorder, and altered sleep structure.
Why symptoms persist is still contentious, however new research set to be presented at this year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) in April 2022, investigates the connection between Post-COVID-19 syndrome, also known as long COVID, and the vagus nerve.
The vagus nerve is the 10th cranial nerve responsible for the regulation of internal organ functions, such as digestion, heart rate, and respiratory rate, as well as vasomotor activity, and certain reflex actions, such as coughing, swallowing and vomiting. This nerve is linked with the parasympathetic nervous system (The Rest and Digest system) which is commonly targeted to calm ourselves.
The study suggests that SARS-CoV-2-mediated vagus nerve dysfunction (VND) could be responsible for many of the symptoms of long COVID, including persistent voice problems, difficulty swallowing, dizziness, abnormally high heart rate (tachycardia), low blood pressure and digestive issues.
With considerations of emerging literature suggesting a disruption of our Autonomic Nervous System (ANS) which is responsible for involuntary regulation of many of our bodies processes such as heart rate, breathing rate and digestion – the Sympathetic Nervous System (SNS) & the Parasympathetic Nervous System (PNS) relationship becomes dysregulated – this is referred to as Dysautonomia.
Due to the interruption in this relationship between these 2 systems, symptoms such as an elevated heart rate upon standing or with light activity may be felt. The inability to control heart rate and blood pressure on changing postural positions. Take for example the change in position from laying down to standing. Blood pools into the lower body which reduces blood flow back to the heart resulting in less blood filling the chambers of the heart (stroke volume). Pressure Receptors (Baroreceptors) in our heart and certain blood vessels detect this change and respond by stimulating the SNS resulting in an increased Heart rate. Our heart is responsible for continually supplying our body and brain with oxygenated blood – this is referred to as Cardiac Output (CO). CO is determined by Heart Rate x Stroke Volume. If one decreases, the nervous responds by increasing the other. For example, as we improve our fitness, our stroke volume improves due to structural changes in our heart (Stronger Muscular Walls). Therefore the heart rate drops as we are able to eject an appropriate amount of blood due to the improvement in stroke volume.
The following table represents how the 2 branches of the ANS affect the Cardiovascular System.
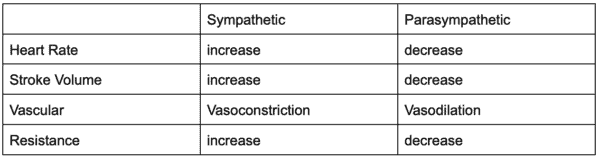
This system is working all the time to regulate essential processes. If the calming aspect of this system isn’t working well, you can understand why an increased heart rate may occur with light activity with long COVID.
In orthostatic (postural) intolerance such as experienced in long COVID, the release of stimulating hormones causes pronounced tachycardia, which is experienced as palpitations, breathlessness and chest pain (common symptoms of ‘long COVID’).
The neurophysiology of what occurs next is beyond the scope of this article, however from a practical point of view of what you should do in the event you are experiencing long COVID is as follows:
- First and foremost, seek professional support if you have declining health.
- Have a graded return to exercise – the BJSM guidelines for returning to training following COVID-19 infection follows a nice simple strategy to return safely to activity. In the event you continue to report headaches of any nature, blood pressure issues, cognitive fatigue, fogginess in the brain or any other concerning symptoms or new symptoms please ask them to seek medical attention for review – https://bjsm.bmj.com/content/54/19/1174
- Dysautonomia can be assessed clinically and strategies can be developed to assist you in your recovery.
- Consideration of postural positions when returning to activity should be considered – for example, upright posture may spike heart rate, whilst recumbent bike may not.
- Consideration of modifying intensity levels based on symptoms. Monitor your symptoms looking for an elevation in symptoms with activity. You will need to have a heart rate monitor on and identify at what heart rate your symptoms spike. For example, if you start training with a headache of 1/10 and it jumps by 2 points to 3/10, at this point you would stop and record your heart rate. You would then look to exercise for the following week or 2 at 70-80% of this recorded heart rate.
May I please make this clear – if you are experiencing ongoing symptoms, don’t push too hard and be kind to your body. Return slowly and drop the intensity. Focus heavily on recoveries with great nutrition, plenty of sleep and hydration.
If you are struggling with persisting symptoms and need support. Please email me at info@kchealthandsports.com.